Superbug hits UK through 'medical tourism'
Updated on 11 August 2010
As a new class of drug resistant superbugs has spread from the Indian sub-continent to the UK via "medical tourism" - a leading expert on infectious diseases tells Channel 4 News it could take ten years to develop an antibiotic to treat it.
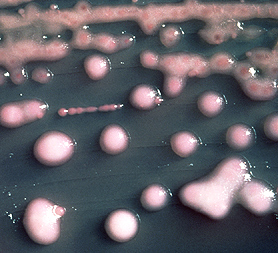
The bacteria - some of which are resistant to all known antibiotics - were unheard of two years ago, but the new study finds evidence they may now be present outside of the hospital setting in the Indian sub-Continent.
There have been around 50 infections caused by the superbug in the UK, and the number is continuing to rise.
At least two people have died in the UK while infected with a strain of the new superbug. However, because these patients were already in intensive care with other illnesses, doctors are unable to say whether the infection was the primary cause of death.
The study found 17 UK infections were in people who had direct contact with India or Pakistan, most of whom had been admitted to hospital there where they probably acquired the infection. Several had gone to India for elective cosmetic surgery.
"It's clear that the UK health service is going to be repeatedly challenged by these infections," says David Livermore, Director of Antibiotic Resistance Monitoring at the Health Protection Agency in London. "It's better that we start trying to control these infections now than when we have thousands of cases."
He said: "We are aware of patients who have died with infections caused by bacteria with this type of resistance. What's much less clear is whether the infection caused their deaths or the patient's underlying disease. This is always very, very difficult to distinguish, where you are dealing with patients who have got severe underlying illness."
The new superbugs were first discovered in India in 2008. A fact reflected in the name of the enzyme that causes their resistance: "New Delhi metallo-ß-lactamase" or NDM-1 for short. "India also provides cosmetic surgery for other Europeans and Americans, and it is likely NDM-1 will spread worldwide," the researchers write in the medical journal Lancet today.
So far they are finding NDM-1 in common gut bacteria like E. coli and Klebsiella pneumoniae. These bacteria can cause urinary tract infections and pneumonia. A short course of antibiotics would normally clear such infections, but carrying the NDM-1 gene turns them from bug to superbug. As such, a normally harmless E. coli infection can be resistant to antibiotics making it potentially life-threatening.
Leading expert into infectious diseases Professor Roger Finch, from the University of Nottingham and Nottingham University Hospital told Channel 4 News it is essential to have an international strategy in place that can invest in new antibiotic drug development or we could face a difficult situation.
Professor Finch said: "Ever since antibiotics were made available drug resistance has been reported; sometimes soon after a drug has been made available; sometimes decades after.
"We've learnt to recognise the problems and make alternative treatment choices. But one issue at the moment is that supply for new drugs has dried up.
"The choice of antibiotics now is frighteningly low. We have two main types in the UK and their use against the NDM-1 enzyme is as yet uncertain territory - one of the drugs is so old, there would be a reluctance to use it on safety grounds.
"So we need an international strategy that can invest in new drug development that is focused on these particular needs so that the industry can gain some reassurance that if a drug is effective and safe, it will have a reasonable return on investment.
"Otherwise we’ll be in the same situation when the next resistant strain occurs."
Professor Finch told Channel 4 News it will take a minimum of ten years to produce a new antibiotic drug that could deal with the NDM-1 enzyme if the superbug takes hold in the UK.
He said: "From experience of similar resistance mechanisms, it could take the next decade to see an increase at a substantial proportion of these drug resistant infections. So we have time to alert healthcare workers, hospitals, GPs and laboratories. It gives us the opportunity to establish effective surveillance systems, internationally, but in the UK we need good surveillance too. To help doctors we need good local surveillance in place.
"Then we need to develop new drugs and rapid diagnostics and that's the problem. New drugs take at least ten years to develop, so if a molecule is discovered today, it won't be until eight, nine, ten years down the line until we could use it as an available new treatment. So it will be a minimum of ten years, and in the meantime we could be in for a difficult situation."
"There are fewer drug companies now investing in anti-biotic research. This is for, they would argue, 'commercial reasons', because it is financially unrewarding, as most are prescribing for generic anti-biotics, (those off-patent drugs that are widely distributable and therefore very cheap).
"So a new drug would be very expensive, would only have a small share on the market and therefore as a business model would be unattractive at this time to the drug companies. There have been many international efforts to address this shortfall – and I'll be attending another one in Sweden in September."
Some of the bacteria sampled from India were found to be resistant to all known classes of antibiotics. A phenomenon called pan-resistance. "A year ago pan-resistance was unheard of," says Tim Walsh from Cardiff University who led the research. But his latest analysis suggests that the superbugs are increasingly common in hospitals in the Indian sub-Continent. Their sampling there also suggests the bacteria may be circulating in the general population which has the potential to speed up spread.
NDM-1 different to MRSA and C.diff
Unlike well-known superbugs MRSA and C. difficile, this new group of bacteria have the ability to pass their genes for antibiotic resistance onto others. From a health point of view that makes them twice as worrying, according to Walsh.
"MRSA can pass from one person to another, but the genetic machinery that causes this new resistance can be passed from one bacterium to another," he says. This gives the genes for resistance "an alarming potential to spread and diversify among bacterial populations".
What worries infection specialists even more, is that drug companies aren't developing new antibiotics. If this new class of superbugs takes hold in Britain it could take many years to develop a new antibiotic to target them. "We could be looking at a dark, ten-year window when we may have nothing to treat these infections with," says Walsh.
It's thought poor controls over antibiotic prescribing in the Indian sub-Continent allowed the NDM-1 gene to evolve. Poor sanitation has helped the bacteria spread from person to person, as well as share the gene, the researchers suspect.
"This research illustrates the relentless evolution and spread of antibiotic resistance genes", says Professor Christopher Thomas, Professor of Molecular Genetics, University of Birmingham.
"It illustrates the importance of considering health issues as a world issue – how antibiotics are prescribed and controlled in one part of the world can very rapidly have consequences elsewhere."
Medical Tourism
In March 2010, Managing Director of Treatment Abroad, Keith Pollard wrote a report entitled "Medical Tourism: Key Facts".
In the report he focused on data collected by the Medical Tourism Survey 2008 conducted by European Research Specialists on behalf of Treatment Abroad.
The data cites Treatment Abroad's estimates into the popularity of medical tourism and why British people travel abroad for treatment.
Medical Tourism: Key Facts - by www.treatmentabroad.com
Treatment Abroad estimates in 2009:
• Around 60,000 UK patients travelled abroad in total. The breakdown was something like this:
• 25,800 dental patients (43 per cent)
• 17,400 cosmetic surgery patients (29 per cent)
• 16,800 for other surgery and treatments e.g. orthopaedic surgery, infertility treatment. (28 per cent)
Source: Projected from the Medical Tourism Survey 2008 conducted by European Research Specialists on behalf of Treatment Abroad. Survey data was obtained from 132 providers of overseas treatment and medical tourism services to UK patients.
Reasons for travelling abroad for treatment
• The most common dental procedures for patients travelling abroad from the UK are crowns, dental implants, bridges and veneers.
• The most common cosmetic surgery procedures for patients travelling abroad from the UK are breast augmentation,breast recution, tummy tuck, liposuction and facelift.
• The most common elective surgery procedures for patients travelling abroad from the UK are hip replacement, knee replacement, laser eye surgery and cataract removal.
Source: Treatment Abroad Medical Tourism Survey 2007/8
UK medical tourists ratings
Treatment Abroad carried out a survey of 650 UK medical tourists, using an external market research company. The results were incredibly positive:
• 97 per cent would go for treatment abroad again.
• 96 per cent would definitely go back to the same provider.
• 96 per cent would recommend it to a friend or relative.
How much can medical tourists expect to save?
Savings of 50 per cent can be achieved, even when allowing for travel and accommodation, according to Treatment Abroad:
• Savings of up to 60 per cent can be made on dental implants, 52 per cent for wisdom tooth extraction and 44 per cent for full acrylic dentures.
• Savings of up to 60 per cent can be made on breast augmentation when allowing for travel and accommodation.
• Saving of 56 per cent on knee replacement by going to India when allowing for travel and accommodation, 36 per cent by going to France.
Source: Treatment Abroad PriceWatch 2009
Read More